The New Era of MS Care: Treatments and Tools Transforming the Future
The Elliot's Neurological Specialties practice combines medical treatments to slow MS progression with holistic approaches to manage symptoms
For decades, people believed that multiple sclerosis was a disease that inevitably led to disability. Today, breakthroughs in treatment and whole-person care are offering patients far more hope and control than ever before. Multiple sclerosis (MS) is a chronic autoimmune disease that affects the brain, spinal cord, and optic nerves, disrupting communication between the brain and the body. While most people associate MS with physical disability, the reality is far more complex and individualized.
“MS is highly individualized, but the underpinnings are that it’s a central nervous system disease,” says Dr. Ann Cabot, a neurologist and MS specialist at The Elliot. “This affects the brain, the spinal cord, and the optic nerves.”
Once diagnosed, typically between the ages of 20 and 50, MS is a lifelong condition. With it, the immune system improperly attacks the myelin that covers neurons. There is currently no cure.
However, over the past two decades, advancements have been made in slowing the disease, reducing relapses, and improving patients’ quality of life. Increasingly, researchers and clinicians are exploring not just how to stop MS progression but also how to better track neurological changes and reverse damage.
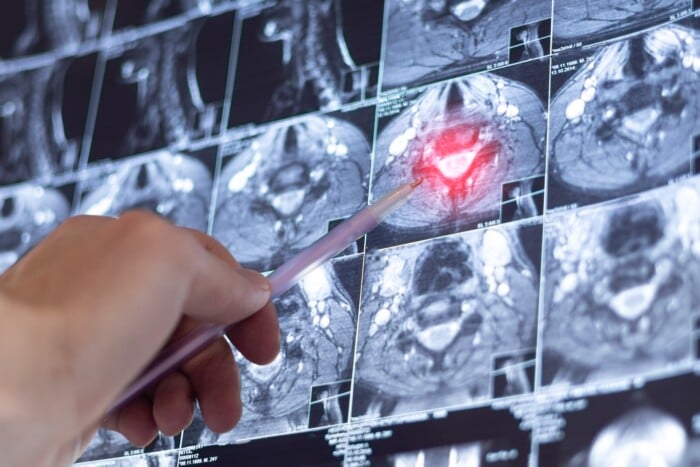
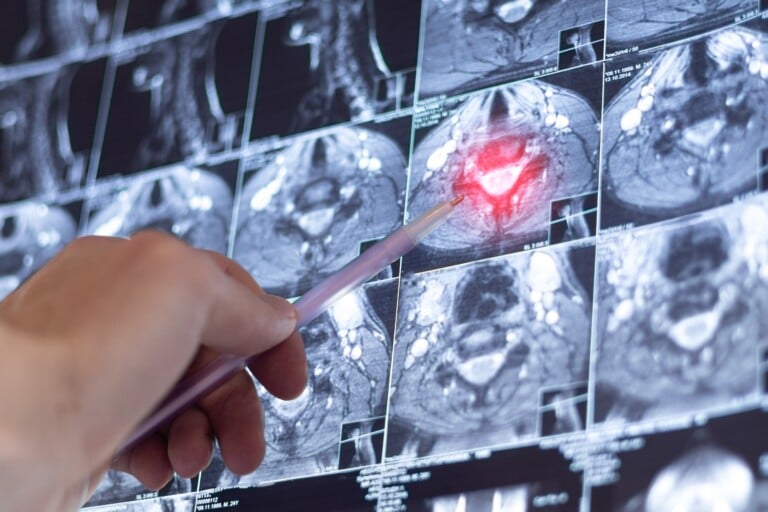
How MS is Diagnosed
Once MS is diagnosed using the McDonald criteria, which includes looking at medical history, doing a clinical exam, using magnetic resonance imaging (MRI), and conducting lab tests, the first treatment is usually intravenous steroids to manage the symptoms. Then, the physician creates an individualized treatment plan with disease-modifying therapies as the foundation of care.
“When I started treating patients, I only had a handful of treatments, and now we have over 20,” Cabot says. “All these treatments have different ways they act on the immune system, side effects, benefits, and risks. The treatments have improved over time, too. We have very high efficacy therapies that we can use to help our patients get their disease under excellent control.”
High-efficacy therapies like natalizumab and B-cell therapies are used to reduce relapses, limit MRI changes, and prevent disabling nervous system damage.
“Research has exploded over the last few decades,” Cabot says. “It’s been a really exciting time to work in this field.”
Whole-person Care at The Elliot
Elliot’s Neurological Specialties practice combines medical treatments to slow MS progression with holistic approaches to manage symptoms.
“My passion is really treating the whole patient, not just to get this disease in check,” Cabot says. “Symptoms are very variable. We utilize a whole lot of physical therapy, physiatrists, and other specialists.”
She notes that coordinated care, from rehabilitation specialists to behavioral health and nutrition services, allows patients to manage MS more comprehensively and sustainably.
The other thing care providers try to encourage is adopting healthy lifestyle habits, including proper nutrition, smoking cessation, regular exercise, and limiting exposure to chemical solvents.
“We know one of the biggest symptoms for patients with MS is fatigue, and we know that exercise can significantly improve a patient’s fatigue,” Cabot says. “It can help them with muscle tone; it can help them with strength; we just have to figure out an exercise program that works for them.”
What’s Next in MS Care
Even with stable MRIs and controlled relapses, some patients may experience progressively worsening symptoms over time. New tools are helping clinicians track these shifts with more precision.
“One thing that researchers are trying to figure out is, ‘what else is a tool that we can use to measure?’ They’re looking at different biomarkers that we can use to monitor disease activity,” Cabot says. “There’s no single perfect tool available yet, but these biomarkers have been extremely helpful. Neurofilament light chain and GFAP are now readily available, and we can use these tools, but I still feel like we’re a little bit in our infancy.”
These biomarkers provide an additional “window” into the activity of the disease and could be used to identify changes before MRI scans reveal them. This is something that patients and clinicians alike have been hoping for.
Also emerging in MS care is remyelination, which focuses on rebuilding the damaged myelin, not just stopping the immune system response.
“Remyelination is a new thing, but it’s definitely a big push in the field. There have been some studies that have failed, and I think when researchers go back, it comes back to the fact that maybe we weren’t really looking at the right thing,” Cabot says. “Combination therapies, or repurposing drugs that are already available for other disease states, may just be a matter of trial and error. What works in a mouse doesn’t always work in a human. Some of the early studies were really exciting, but didn’t seem to pan out yet, although I’m still very optimistic they will be able to find that.”
Remyelination treatments may one day be able to restore lost function, providing a degree of healing that was previously thought to be impossible.
Support Beyond Medication
While it can be overwhelming for patients to face the prospect of a lifelong neurological disease, they have more options for care than ever. When existing high-efficacy or emerging therapies are paired with holistic wellness services, patients can work with their physician to create a treatment plan that may include support groups, nutrition guidance, and physical therapy to address any needs they have.
A significant change in MS care is the focus on improving overall quality of life. This combination of support and medical innovation reflects a broader shift toward treating the whole person and not just the illness – something that has always guided how clinicians at The Elliot support patients.
“Do I have a magic wand? No, but at least we can point our patients in the right direction toward resources that can be very beneficial,” Cabot says. “We’re really lucky at The Elliot, because we have so many resources for the patients that they can utilize to help with their wellness.”
As research accelerates and therapies evolve, Dr. Cabot emphasizes one message for patients: MS is a lifelong condition, but it does not have to define your life. With the right tools, team, and support, people with MS can continue to live fully and thrive.
If you or a loved one is living with MS, The Elliot’s Neurological Specialties team is here to help. Learn more at ElliotHospital.org/MS