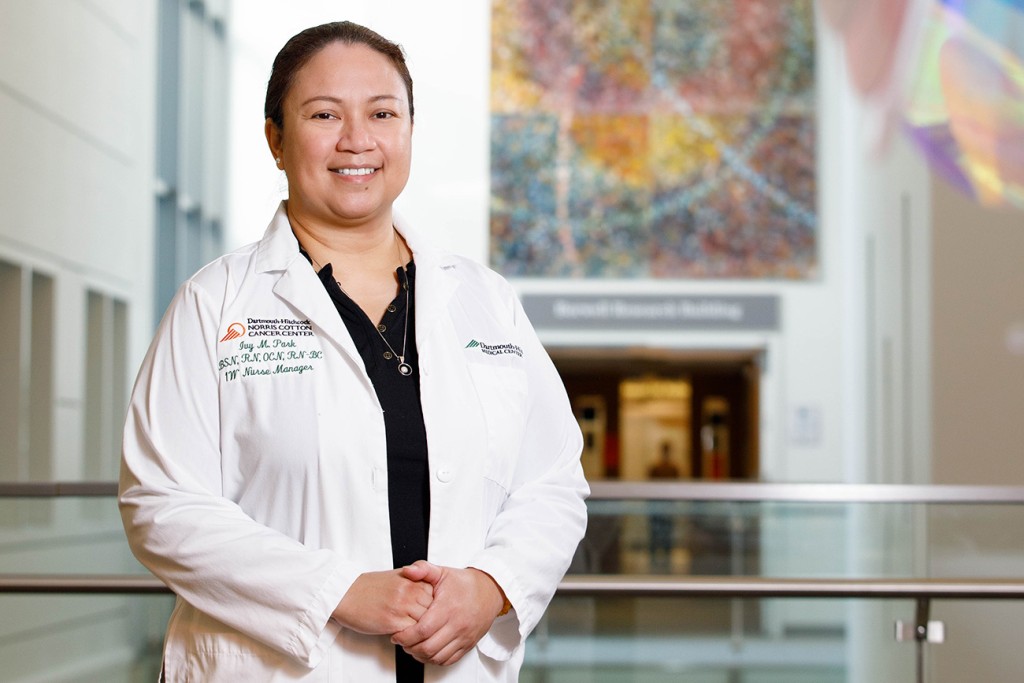
Excellence in Nursing Awards 2025
Too often, nurses are the unsung heroes of medicine. In fact, they are key members of any health care team, but their skills and contributions go unrecognized time and again. As the world continues to come back to baseline post-pandemic, the public has become more aware of the challenges nurses face, and the professionalism and compassion they demonstrate as they continue to provide the best possible care in stressful, uncertain times.
New Hampshire Magazine, in partnership with the New Hampshire Nurses Association, is proud to celebrate the important contributions by nurses and their many talents with the eighth annual Excellence in Nursing Awards. This past winter, we accepted nominations for New Hampshire nurses in 18 vital specialties, from pediatrics and public health to leadership and education. The winners were selected by an independent committee of nursing leaders from adjoining states.
Each nurse profiled represents the very best in nursing — those who go above and beyond to comfort, heal and teach.
C atherine Amarante, BSN, RN, GERO-BC
atherine Amarante, BSN, RN, GERO-BC
Dartmouth Health Lead, Honoring Care Decisions
Gerontology Nursing
Dartmouth Health
Catherine Amarante, a board-certified gerontological nurse at Dartmouth Health in Lebanon, helps provide direct care for older adults, including those with dementia and their care partners. She also teaches, mentors and helps with transitions of care.
She began as a community nurse for families and children in Brattleboro, Vermont, more than 25 years
ago. But after working per diem in a nursing home, she discovered that helping older adults was her calling.
“I work in a variety of ways to improve the care of frail older adults, particularly persons living with dementia, and their care partners by providing direct care, teaching and mentoring, assisting with transitions of care and ensuring goal-concordant care by eliciting what matters most to each individual,” Amarante says.
Amarante says students, novice and nursing assistants, and hands-on caregivers motivate her.
“I am inspired every time I see that light go off, when a new nurse puts together a complex assessment and understands what they need to do next, when an LNA has success helping a person living with dementia who is struggling, and every time a caregiver experiences true connection and joy with a patient,” Amarante says.
 Jennifer F. Winslow, MBA, MSN, APN, FNP-BC
Jennifer F. Winslow, MBA, MSN, APN, FNP-BC
Associate Director for Patient Care Services
Chief Nursing Officer Senior Nurse Leader (Small)
VA Manchester Healthcare System
As chief nursing officer at VA Manchester Healthcare System, Jennifer Winslow provides executive oversight of clinical and administrative teams, including nursing, pharmacy, social work, education and sterile processing.
Winslow became a nurse because she wanted to make a meaningful, positive impact on people’s lives. She began her career 30 years ago as direct care nurse on a busy medical-surgical unit in New York. Since then, she has served as
a nurse practitioner and in multiple administrative leader-ship roles.
“Regardless of the position, my purpose has stayed the same: to uplift, support and improve the lives of those around me,” Winslow says.
Her transition from the private sector to the Department of Veterans Affairs was inspired by her father, a veteran of the Korean War.
“For years, he spoke of the exceptional care he received through the VA and encouraged me to consider becoming part of that mission-driven team,” she says. “He was right. The VA’s commitment to serving those who served is truly unparalleled.”
Winslow considers integrity and trust essential to effective leadership.
“A CNO must set the tone for an ethical, accountable nursing culture by building authentic, trusting relationships and inspiring, influencing and motivating their teams,” she says.
 Amber Bechard MSN, RN, CNL, TCRN
Amber Bechard MSN, RN, CNL, TCRN
Trauma PI Coordinator
Nurse Innovator
The Elliot
Amber Bechard began her nursing career 20 years ago and worked a large part of her career in the intensive care unit. She pivoted to the trauma program five years ago, where she now monitors and evaluates the care of the patients, helps identify areas for improvement and implements changes to improve outcomes and comply with quality standards.
Bechard is honored to be a part of developing and implementing new approaches to help her team, one of which involved the improvement in administration of blood products with a goal to standardize the process and reduce waste.
“I organized and developed an education plan that included nurses from the emergency department, PACU and ICU,” Bechard says. “As part of the training, we performed a relay-style activity where teams raced to administer large volumes of blood products accurately and efficiently.
Nurses worked alongside colleagues from other departments, she says, encouraging collaboration and building a stronger sense of teamwork across the hospital.
“As a result of this initiative, our staff reported increased confidence in massive transfusions, and we have observed a reduction in the blood product wastage,” Bechard says. “The feedback was extremely positive, and this approach is now being used as periodic training throughout the hospital.”
 Johanne Fisher BSN, RN, CPN
Johanne Fisher BSN, RN, CPN
Pediatric Nurse
Pediatric and School Nursing
Elliot Hospital
As a mother of two and pediatric nurse of 13 years, Johanne Fisher’s kids inspire her to pursue excellence in her field daily.
“I frequently find myself thinking how I would want my children to be cared for and how I would want to be cared for as a parent of a hospitalized child,” she says. “This allows me to be truly empathetic and meet the needs of my patients as well as the families I care for.”
She is also encouraged by one of her co-workers, a longtime pediatric nurse of over 35 years.
“I always tell her that she would be the nurse I want caring for my children if they were ever hospitalized,” Fisher says. “She cares for her patients as if they are family, and this is something that you don’t find all the time.”
Empathy, creativity and compassion are the key characteristics that are needed in her field, she says.
“You frequently have to flex to meet the developmental needs of your patients, and this is what makes pediatric nursing so unique. We care for such a wide age range and constantly must be creative in creating a safe, fun and therapeutic healing environment for our patients and families.”
 Pam Switzer MSN, BS, RN
Pam Switzer MSN, BS, RN
Nurse Manager
Frontline Leader (Large)
Cheshire Medical Center
Pam Switzer is a nurse manager for the preoperative unit and the post-anesthesia care unit at Cheshire Medical Center in Keene. Part of her job includes ensuring safe interventions when patients are under anesthesia or sedation. Switzer also manages the business and financial plans and the daily operations for both departments.
But nursing was not Switzer’s initial career. For a time, she worked in medical research, using her B.S. in physiology and neurobiology. Then, after volunteering as an EMT, she began to realize her true calling: helping people. After feeling “helpless” when her grandmother needed medical care, she decided she never wanted to feel that way again.
“I enjoy helping others and have a passion for high-quality and safe care,” Switzer says. As she favored bedside and ICU nursing, being a leader wasn’t on her radar until a mentor suggested she consider nursing leadership.
“She saw something in me I had not even known to look for,” Switzer says.
A nurse since 1995, Switzer then went back to school to obtain her master’s in nursing leadership, “to make sure I was best equipped to support my teams.” Switzer says her family is the reason she works so hard to provide the utmost care for her patients.
“We care for people at their most vulnerable times,” she says.
 Chastity Hodgson RN, BSN, TCRN
Chastity Hodgson RN, BSN, TCRN
Charge Nurse
Emergency Nursing
Cheshire Medical Center ED
After her sister was born with multiple orthopedic complications, Chastity Hodgson spent her young adult life being an EMT wanting to serve those around her.
Her passions led her to a summer working in the ER where she realized how much she loved the skills nurses were able to use and the impact they had on their patients. She applied to work at the Chesire Medical Center’s Emergency Department in 2018, and she’s been there ever since.
Her day-to-day includes triaging patients, managing the flow of the department, assisting the team in any way she can and finding solutions to many types of problems as they arise.
This fast pace has been hard to get used to over the years, but she uses it to fuel her days, both good and bad.
“Being a charge nurse that the entire team can not only rely on in every aspect of the job every day, but also someone that they want to work with, is what I strive to be,” she says. “Being able to make the days of others just a little bit easier pushes me to work harder.”
 April Phelps DNP, RN, CNL
April Phelps DNP, RN, CNL
Director, Clinical Assistant Professor
Public Health Nursing
UNH Nursing
April Phelps oversees UNH Nursing’s Direct Entry Master’s of Nursing Program, which is designed to ensure talented nurses enter the workforce “equipped with a commitment to compassionate and evidence-based care.”
Additionally, as the health officer for the town of Fremont, Phelps identifies and responds to public health threats. In high school, Phelps decided to join the Army so she could become a nurse — a choice her mother was hesitant to endorse.
“She exclaimed, ‘No, my baby is going to go off to war!’ I reassured her, ‘Mom, they’ll pay for my bachelor’s in nursing.’ Her reply? ‘Where do we sign up?’”
After earning her BSN through Army ROTC in Portland, Oregon, Phelps began her nursing journey in 2000 as an Army nurse at Landstuhl, Germany, working in a maternal child unit. She considers the ability to take initiative and make difficult decisions one of the most important character traits in nursing.
Phelps says she finds inspiration daily from the determination and passion of her students.
“I have had the honor of caring for military service members over the years who have inspired excellence,” Phelps says. “My husband, son, family and friends provide steadfast support, helping me persevere through challenges to strive for excellence throughout my career.”
 Eileen Glover DNP, MSN, RN-BC, NEA-BC
Eileen Glover DNP, MSN, RN-BC, NEA-BC
Department Chair, LPN Program Director, Nursing Professor
Professional Nurse Educator
River Valley Community College
Eileen Glover came to nursing later in life, graduating at 38 with an associate of science degree in nursing at River Valley Community College in Keene, where she now serves as professor of nursing and department chair of Allied Health.
Most of her time is devoted to the LPN program. Prior to arriving at RVCC, she spent her nursing career at Brattleboro Retreat in Vermont, working in every nursing role, ultimately rising to chief nursing officer.
“In my time there, I helped create then run the first (and only at the time) in-patient unit for LGBTQ+ patients,” says Glover, who obtained her master of nursing education in 2014 and completed her doctor of nursing practice in executive leadership in 2018.
Glover has presented at local, national and international conferences about LGBTQ+ health, and in 2016 published an article in a peer-reviewed nursing journal about mental health and addiction issues in the LGBTQ+ community.
She finds her greatest inspiration from her students.
“They are overcoming so many obstacles to achieve their goals, and we are honored to be a part of their journey,” Glover says. “I want to be remembered as the person who helped them see that they can (and will) achieve great things in their lives.”
 Christine Gooley RAPRN, BC
Christine Gooley RAPRN, BC
Adult Nurse Practitioner, Department of Infectious Disease
Advanced Practice Nursing
Dartmouth Hitchcock Medical Center
Christine Gooley has always had a heart for caring for HIV/AIDS patients. Her desire led her to many years of teaching related to HIV/AIDS, counseling related to exposures, and using the rapidly expanding number of medications both for HIV treatment and prevention.
Now, she is a part of the outpatient IV antibiotic team at Dartmouth Health, where she helps treats all kinds of infections from osteomyelitis to endocarditis, and she helps to make sure patients have a smooth transition from being in the hospital to going home or to a rehab facility with IV antibiotic therapy. She also checks in with patients for telehealth calls and sees them in their clinic to make sure the infection is cleared.
Humor is necessary in her day-to-day work to lessen the patient’s burden of illness and disease, but so is attention to detail.
“It’s crucial to follow culture results and the microorganism sensitivities to antimicrobials so that the treatment plan works,” she says. “Patients with serious infections who are on long-term antibiotics must be watched closely for side effects or toxicities of the medications, in addition to favorable response to the treatment. There are a lot of moving parts to a comprehensive treatment plan, and having attention to detail has served me well.”
 Justin Montgomery DPN, APRN
Justin Montgomery DPN, APRN
Vice President Nursing
Academic Nurse Educator—Researcher
Dartmouth Hitchcock Medical Center
While reflecting on his nursing career, Justin Montgomery believes that the most essential characteristic to nursing is authentic curiosity.
“You need this in investigating clinical questions, operational challenges and exploration of new approaches for delivery of nursing care,” says Montgomery, who is now the vice president of nursing at Dartmouth Hitchcock Medical Center, adjunct faculty at Colby-Sawyer College and instructor at the Geisel School of Medicine.
Since joining the Air Force out of high school, Montgomery has served as a firefighter, working as a flight communicator for DHMC and now has a long professional journey in academic, clinical and leadership domains.
Not a single story could capture his gratitude for moments of connections with students and patients over the years, but one particular story comes to mind, he says.
“A few years into my career, I had a mentor who took a chance on me by providing an opportunity to teach principles of evidence-based care for geriatric patients,” he says.
Montgomery was humbled by the opportunity and asked how he could ever repay her mentorship.
“She responded, ‘You can’t. You can only pay it forward.’ I’ve worked tirelessly since that conversation to pay it forward. It’s the least I can do for all I have received.”
 Jennifer Thebodeau MSN, RN, CCCTM
Jennifer Thebodeau MSN, RN, CCCTM
Pact RN, Primary Care
Ambulatory Care Nursing
VA Manchester Healthcare System
After being honorably discharged as a hospital corpsman in the Navy, Jennifer Thebodeau obtained her nursing degree and became a champion for coordinating complex care for chronic illness and post-hospital discharges.
After 15 years of serving the local community and growing in her profession, Thebodeau knew that it was time to make do on a promise to herself to help her fellow veterans and joined the Manchester VA Medical Center.
She uses the skills she has built over the years to take care of her patients, including ensuring that their transition home after a hospital stay is as comfortable as possible.
“I work with other members on a patient’s care team to assist with needs that arise just before and after a person returns home,” she says.
During the first few days after a veteran patient returns home, Thebodeau checks in with them to assess what other care they might need.
“I will work with social workers, rehabilitation facilities, discharge planners, caregivers, other nurses and providers — sort of like the hub pulling the patient care team together — for a positive patient recovery from their hospital or rehabilitation stay,” she says.
“This process and the patients involved in them inspire me every day. We can always improve if we just use those lessons to grow our talents and skill set in nursing.”
 Nicole Wakeman BSN, RN
Nicole Wakeman BSN, RN
Clinical Manager of Inpatient Services
Frontline Leader (Small)
New London Hospital
After being a stay-at-home mom of nine kids for 21 years and advocating for her children who had various medical diagnoses, Nicole Wakeman decided to become licensed in the field that was already woven into her life.
She spent her 40th birthday attending River Valley Community College’s LNA program. Now she oversees the day-to-day operations and coordination of patient care for the medical/surgical unit and the special care unit at New London Hospital.
While her mom, who was also a nurse, and her kids inspire her every day, it’s Wakeman’s fellow staff who encourage her to excellence in her position.
“Seeing how tirelessly they work every shift pushes me to ensure I am providing them with every resource, support and tool necessary for them to be a success,” she says. “If they’re expected to show up in a snowstorm, I will be showing up in a snowstorm (even though I could work remote).”
If her team’s equipment is breaking down, they work together to investigate newer options and what would be best for them and the patient population.
“I measure my success by how successful they are,” she says. “Their dedication to our patients and each other is what inspires me to do my very best in providing for them.”
 Ellie Atherton, DRN
Ellie Atherton, DRN
Hospice Nurse
Hospice-Palliative Care
Granite VNA
In 2003, while focusing on hospice care during her last semester of the nursing program at Manchester Community College, Ellie Atheron was assigned to a hospice rotation.
“On the first day, I knew hospice was going to be my career path. Twenty-two years later, I’m still caring for the dying, supporting their families, and I feel honored to walk alongside them until they reach the end of life.”
At Granite VNA, Atherton gives comfort-focused care to those with life-limiting diseases and offers families the emotional support they need. Atherton lists compassion, authenticity and the ability to be present as vital characteristics when caring for patients.
“I don’t take my role in caring for the dying lightly, because I am present during some of the most private and emotional times of their lives. Honoring patients’ wishes to do things their way until the last breath of life inspires me to be a great advocate,” Atherton says.
Atherton is reminded daily of the concerns of those who will soon leave behind their loved ones.
“Patients have taught me that forgiveness and love are the balance that allows for less suffering in life and the opportunity for a peaceful death,” Atherton says.
 Tracy Galvin DNP (c) MSN, RN, NEA-BC
Tracy Galvin DNP (c) MSN, RN, NEA-BC
Chief Nursing Officer
Senior Nurse Leader (large)
Dartmouth Hitchcock Medical Center
This May marks two years that Tracy Galvin has been the chief nursing officer for Dartmouth-Hitchcock Medical Center in Lebanon, but her career stretches back decades.
“I started as a new graduate from Northeastern University in 1987 at Lahey Hospital and Medical Center. I was with this organization for 36 years and had been the CNO for eight years before I left,” Galvin says.
Her experiences as a nurse over the years has enriched her life in more ways than she could imagine.
“There are so many stories to share, from my direct care work to my leadership roles, that I could write a book. Some are more memorable than others, but all have helped me to become the leader I am today.”
Galvin says flexibility and being able to roll with the punches are important tools to have as a nurse.
“In the role of the CNO or any nurse leader, you have to be able to adapt to change and work with the resources that are available,” Galvin says.
Galvin also credits her mother, who was also a nurse, as her inspiration for the myriad accomplishments in her life. “I always know I wanted to be a nurse because of her,” she says.
 Lauren Kempton BSN, RN-BC
Lauren Kempton BSN, RN-BC
Fitch Unit
Medical Surgical Nursing
The Elliot
Lauren Kempton comes from a long line of nurses, and when she completed high school, she knew exactly what she wanted to do.
“I have always felt it was my calling to continue in their footsteps and went to nursing school right after finishing high school,” she says.
After graduating with her BSN at Fitchburg State University, Kempton got her foot in the door right out of college as a nurse in New Hampshire with a medical-surgical unit that was willing to train her.
“I applied for a nursing position on the Fitch unit at Elliot Hospital after seeing it was a general medical floor that also had a population of oncology/hospice patients,” she says. “My goal was to get a year or two of experience before possibly transitioning into a new specialty. Little did I know my ‘one or two-year plan’ would evolve into me now entering my 11th year as a nurse on Fitch!”
Kempton continues to find inspiration through her love of training new grads and taking on a mentorship role for them.
“I believe having trust and open communication is so important to support an environment that new grads can grow and develop their critical-thinking skills in and remain calm in a fast-paced and constantly changing environment,” Kempton says.
 Jill MacGregor MSN, APRN, FNP-BC
Jill MacGregor MSN, APRN, FNP-BC
Family Nurse Practitioner
Psychiatric and Mental Health Nursing
Center for Recovery Management at Nashua
As a nurse practitioner at the Center for Recovery Management in Nashua, Jill MacGregor engages with patients to explore evidence-based approaches to support their recovery goals and overall wellness.
MacGregor completed undergraduate studies in health promotion and disease prevention at Pennsylvania State University. She pursued graduate studies at the MGH Institute of Health Professions, where she started her career in nursing. In 2009, she became a family nurse practitioner working in primary care.
In 2018, she began treating patients with substance use disorders and in 2020 joined the Center for Recovery Management in Nashua.
Compassion is essential in all areas of nursing, but especially in behavioral health and addiction medicine.
“It begins with actively listening to patients and thoughtfully
considering their concerns to build trust and respect,” she says.
MacGregor recalls a young man grappling with addiction who revealed to the medical team that he had just become a father and wanted to become sober.
“While his initial motivation was solely for his son, he eventually realized he needed to fight for himself as well,” MacGregor says. “He regularly visited the office for follow-up appointments, and one day, he proudly announced that he had been sober for a year and had just celebrated his son’s first birthday!”
 Pamela Bullock RN, BC, BSN
Pamela Bullock RN, BC, BSN
Medical Surgical, Nurse Clinical Supervisor
Nursing Informatics
Littleton Regional Healthcare
Pamela Bullock is a jack of all trades who wears many hats, but from a broad view, she supports the nursing staff and providers with EMR concerns and issues, including training all incoming nursing staff that work on her hospital side of their health care system.
She also works as a clinical supervisor to keep her clinical skills and knowledge current, and has been known to pick up an occasional shift on the medical surgical unit with direct patient care, when needed.
Of all the hiccups that may pop up throughout the day, the challenges of the electronic record will always be the most frustrating, she says.
“What gets you through is Laffy Taffy and a good group of friends that understands the complexity of making changes to an EMR,” she says. “I will always remember the good times our condo nursing team had as we built our first EMR.”
Bullock enjoys facing new challenges and learning how to navigate them.
“I love that I am one of the first people that interacts with our new employees and students training them on the EMR, and I love the fact that I can help individuals who may be struggling with some aspect
of documentation,” she says. “As frustrating as they are, it’s the challenges that force me to problem-solve and find a solution to help myself and my team.”
 Nurses of NH Hospital
Nurses of NH Hospital
Award of Merit
NH Hospital
The staff at NH Hospital went through the unthinkable on Nov. 17, 2023, when a gunman opened fire in the lobby, killing Bradley Haas, a security officer for the Department of Safety. In the years since, New Hampshire has worked to improve security in state buildings, but the marks on staff members like nurse specialist Abigail Barrette remain.
“You never think an event like this would ever happen in your lifetime, let alone at your work where healing should be occurring,” Barrette recalls. “I am eternally grateful for my colleagues that day. We worked like a well-oiled machine, not allowing our emotions to affect the care we were providing to our patients, who were understandably frightened. I feel we all have a deeper appreciation for everything that each discipline does daily, like carrying on despite the uncertainty of what each day might bring.”
Healing has come in many forms for Barrette and her colleagues since, like having comfort dogs at the hospital, extra meetings with supervisors, and self-care and therapy when needed. “As my own supervisor has always told me, you can’t pour from an empty cup,” Barrette says. “You can’t give the care and compassion you would like to when you have not shown yourself the same.”
Caring for patients inspires Barrette and her team to keep moving forward.
“Never forget that whether large or small, you make a difference in your patients’ road to recovery and wellness,” she says. “Each interaction can instill hope when someone may have none or remind them of the reason that the world needs them here.”